Why Walk Again post stroke?
People who walk after stroke live longer, live better, live healthier
“The regaining of walking ability is one of the main goals of rehabilitation following stroke.”
Matjacic et al., rehabilitation researcher
A stroke can damage the brain in minutes, potentially robbing the survivor of many skills that previously were taken for granted. Among the precious things lost — at least initially — may be the ability to walk.
Stroke is a leading cause of long-term disability. Impairments resulting from stroke lead to persistent difficulties with walking. For a stroke survivor, learning to walk again should be a top priority.
Ambulation is a crucial component to recovery and lifetime health. Movement keeps joints lubricated and stimulates your brain. Stronger muscles and bones provide the strength and balance you need to be active.
After stroke, physical activity is important to not only to regain motor and cognitive function, but to also help ward off another stroke. Walking again is one step towards that goal.
Walking after a stroke: recovery is possible
Walking ability has important health implications, providing protective effects against secondary complications common after a stroke such as heart disease, musculoskeletal issues, and systemic disorders.
Even if someone has been primarily wheelchair or bed-bound for years, with little intervention, they can achieve significant results and greater quality of life with the proper program, and with proper equipment.
Many of our GHSII clients see consistent standing and walking progress in the months, years, or even lifetime of recovery. The brain has significant potential to do, adapt, and change, even years after a stroke.
Why is walking affected by a stroke?
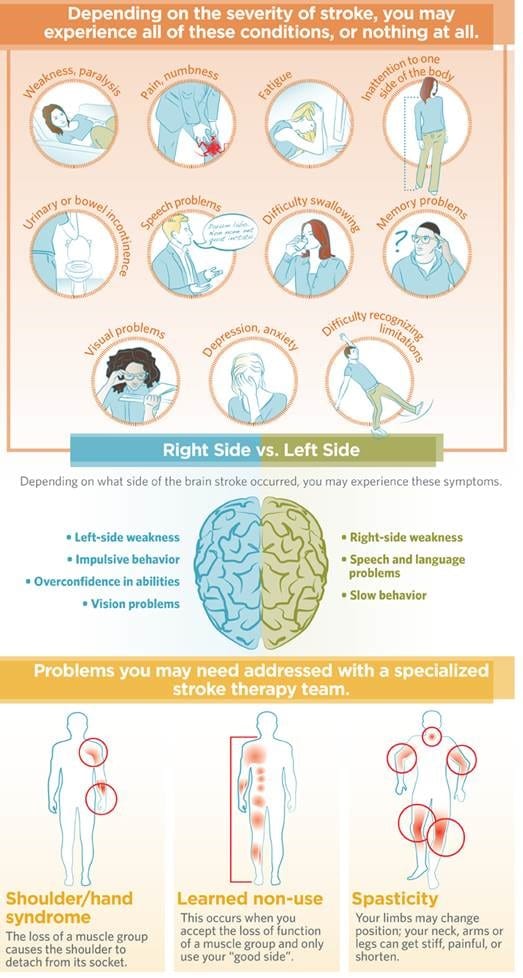
Many strokes injure the motor fibers connected to movement. Typically strokes damage portions of one side of the brain and affect the opposite side of the body. A stroke can make one side of the body weak or paralyzed, making it difficult or impossible to walk.
A patient’s balance may be shaky if the cerebellum (the part of the brain that controls equilibrium) is injured. Along with paralysis, weakness, numbness, and loss of balance, many stroke patients are left with distorted perceptions about where their body ends.
Injury to the motor portion of the brain can also diminish muscle tone and control, another obstacle to walking. Muscles can lose the ability to contract altogether or, on the contrary, become overly contracted and too rigid to allow a simple walking motion.
How does a stroke survivor learn to walk again?
A patient’s rehabilitation should start as soon as he or she is stable. This could mean within 24 hours to a few weeks or longer. Established guidelines, as well as a huge body of literature, insist that the earlier therapy is initiated the better.
Before walking begins, a practitioner may guide the patient through pre-walking exercises to ready other pertinent muscles. If a patient’s trunk muscles were affected, causing him or her to lean to one side or to the front, therapy may start with core strengthening exercises in a sitting position.
The next step might be to work on standing until the patient feels anchored and secure. Learning to walk again involves scores of muscles and many isolated movements. Caregiver/practitioner and patient should approach the complex act of learning to stand and walk again in a safe, supported manner.
Physical activity remains a cornerstone in risk-reduction therapies for the prevention and treatment of stroke. Regardless of how a stroke survivor learns to walk, one thing is certain: the stroke survivor needs to get moving.
The months or years of recovery may seem overwhelming, but survivors need to keep in mind that the potential for progress is always there.
Early intervention is key
There is growing evidence showing the provision of early ambulation support to critically ill and injured patients result in more favorable recovery outcomes as compared to less aggressive approaches.
A recent study at Cleveland Clinic found that patients participating in early mobility routines after neurological injury recovered quicker and went home earlier than those receiving standard care.
Evidence based practice confirms that ambulation spanning the acute through long-term stroke recovery phases using an over-ground, all-in-one standing frame and walking frame support system, such as the Gait Harness System®, should be encouraged. Functional recovery progress may then be made immediately, and in the months and years to come.
Overcoming risks
Stroke survivors who return home after undergoing rehab are often wary of walking or exercising due to fears of falling — a fear that can lead to them being stuck in the house.
Impairments resulting from stroke, such as lack of energy, muscle weakness, pain, spasticity and poor balance can lead to a reduced tolerance to activity and further a sedentary lifestyle.
Immobility-related complications are very common in the first year after a severely disabling stroke. Patients who are more functionally dependent in self-care are likely to experience a greater number of complications than those who are less dependent.
Bone mineral is lost during immobilization. Sitting for more than 8 hours a day has been shown to negatively impact health and mortality. Standing and walking again are the recommended healthier alternatives.
Neuroplasticity
Traditionally, treatment has focused on adaptation, or learning to live with the resulting impairments. However, considering incoming research and evidence based reports, many practitioners, caregivers, and clients are looking at the opportunity for recovery.
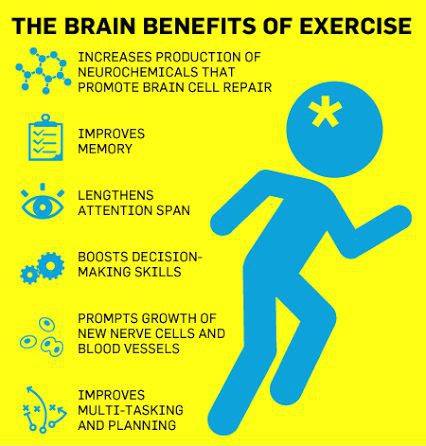
Neuroplasticity is the term that describes the brain’s ability to reorganize by forming new neural connections necessary for recovery. Engaging in an active standing and walking process sends messages back to the brain, until the movement is relearned. We are starting to realize there is more potential for recovery of the brain, and that recovery is not limited to the early days or months post stroke.
The right exercise, for the right duration, at the right time, can promote neurotrophic growth factors. Products and treatment techniques can be implemented with this in mind.
This should be done not only with specific rehabilitation intent, but also with a whole-body focus. Cognitive, emotional, psychological, and physiological processes are intertwined. Improvement in one area tends to bolster improvement opportunities in other areas.
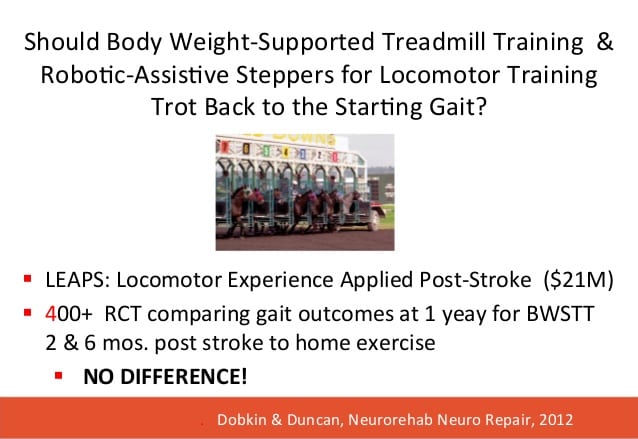
Over-ground therapy is more effective than robotic BWSTT
Over-ground walking is an effective means to regain greater independence of gait. The Gait Harness System® provides a secure, comfortable, safe environment for the neurological client to practice functional standing and walking again.
Body weight support treadmill training (BWSTT), which relies on total guidance of robotics, leaves little room for active effort on the part of the client, a key aspect in motor learning and functional gains.
Research shows that for most participants, BWSTT is not sufficient to induce long-term improvements in balance and balance confidence. Additionally, a recent study confirmed that “Body weight–supported treadmill training is no better than over-ground training for individuals with chronic stroke.”
Comparing over-ground training to the robotic treadmill training suggests that it is not the length of time spent in training, but rather how an individual engages in the activity that produces the results. Or, that a greater number of step repetitions produces greater functional change in walking ability, but only when transferring the skill to a natural walking environment.
In stroke survivors living in the community with marked limitations in walking, treadmill training with BWSTT was not shown to be superior in improving the functional level of walking to home administered physical therapy focused on less-intensive but progressive strength and balance training.
Studies also show that walking on a treadmill does not carry over well to over-ground walking. The active motor requirements in over-ground walking appear to be an important factor for promoting spatial symmetry in gait.
Compared to BWSTT, a recent study showed that step-length symmetry ratio improved only with the over-ground therapy gait group. Reduced step length symmetry ratio has been found to increase fall risk. Improving step length symmetry through over-ground gait training has the potential to decrease fall risk.
As individuals with stroke often desire to look more “normal” when walking, improving gait symmetry through over-ground practice, in the “real world,” contributes to that goal.
The Second Step GHSII encourages client-centered, supported, faster walking and more functional, natural movement. The System provides a novel, optimal gait training strategy for post stroke survivors, enabling goal-directed recovery and maintenance of walking ability.
Ready, set, walk!
With proper practitioner/caregiver support and safe therapy equipment, stroke survivors can reduce high risks for falls, fractures, learned non-use behavior, and further declines in mobility.
Walking speed predicts the level of disability. Regaining independent ambulation, and increasing walking capacity, is a top priority for individuals recovering from stroke. Thus, physical rehabilitation post-stroke should focus on improving walking function and endurance.
However, often the amount of walking completed by individuals with stroke attending rehabilitation is far below that required for independent community ambulation. Increased walking activity with supportive equipment such as the Gait Harness System II can improve walking function and community re-integration.
Beginning to walk again, even long after a stroke, has been associated with functional gains.Taking a brisk half-hour walk outdoors three times a week can significantly boost stroke survivors’ physical fitness and improve their ability to get around — all within just a few months, new research from Stroke, a journal of the American Heart Association, shows.
Repetition, intensity, practice: it takes willpower
How do stroke survivors move beyond the obstacles of learning to walk again? Through sheer determination and a mindset of never giving up, no matter how long it takes: repetition, intensity, and practice.
Studies show a daily commitment to standing and walking therapy practice (or ideally multiple therapy sessions daily) yields the best outcomes.
Typically, the amount of walking completed by post stroke individuals attending rehabilitation is far below that required for independent community ambulation. Increased walking activity after discharge from rehab will improve walking function, physiological condition, psychological health, psychosocial connection, and community re-integration.
Evidence supports the impact of home-based supported standing and walking programs on range of motion and exercise activity. 60 min of standing and walking practice daily is suggested for mental function and bone mineral density. The Second Step GHSII provides a unique, safe combination of standing frame and walking frame benefits for stroke survivors who need the extra support.
Many people think after a certain number of years, they’re not going to make progress. Research shows that is simply not true.
Walking again enhances life quality. Every step forward is progress. Eventually, even some stroke survivors who believe they’ll never walk again experience great improvement.
Resources
https://www.secondstepinc.com/walk-again-post-stroke
https://www.secondstepinc.com/stroke-survivor-gallery
References
National Stroke Association 800-STROKES (800-787-6537) http://www.stroke.org
Post-Stroke Rehabilitation Fact Sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Pa…Fact-Sheet
Gorden NF, et al. Physical activity and exercise recommendations for stroke survivors. AHA scientific statement. Circulation April 27, 2004.
https://www.ncbi.nlm.nih.gov/pubmed/15117863
Learn more about Second Step products at https://www.secondstepinc.com/products
Contact usto request a free quote
Questions about the Second Step Gait Harness System®? Call us at 877.299.STEP (7837), visit our website ator Contact us Today at
Now people can get the help they need to stand and walk again. Visit to find out more about the results oriented, clinically proven Second Step Gait Harness System® (GHS) and NEW Gait Harness System® II (GHSII).
Since 1989 the Second Step GHS has been the durable standard of excellence in commercial grade rehab standing frame and walking frame equipment. The GHS provides new therapy opportunities to walk again, even for those who have not walked in years, helping people regain healthy functioning after stroke, brain injury, cerebellar degeneration, spinal cord injury, orthopedic, neurological, lower extremity amputation, Parkinson’s, Alzheimer’s, and other ambulation, gait and balance rehabilitation issues. The GHS is more than a standing frame, walking frame, gait trainer or walker.
The GHS is used world-wide not only in outpatient and inpatient clinics, but also in the home. Discover how Second Step is “Helping People Walk Again” by keeping users, caregivers and practitioners safe, and simultaneously facilitating healthy, functional therapy outcomes.
Follow us on Facebook: https://www.facebook.com/secondstepinchelpingpeoplewalkagain/